
Male Reproductive Toxicology
The potential contribution of environmental chemicals to endocrine modulation in exposed humans and the subsequent impairment of fertility is one of the most intensely, and controversially, discussed questions in contemporary human toxicology research. This project aims to support regulatory authorities by developing scientific expertise which will contribute to national and international efforts in addressing underlying mechanisms leading to adverse effects on male fertility.
The incidence of male reproductive disorders such as urogenital malformations and testicular cancer is rising in several countries. In Switzerland, as in many other countries sperm counts in young adult men are declining and additionally Switzerland has one of the highest testicular cancer rates in Europe.
Many compounds have been proposed to induce testicular dysfunction and subsequent reproductive disorders by disrupting endocrine functions – including phthalates, organoplatinum compounds, organotins, heavy metals, vinclozolin, and other pesticides. However, the underlying mechanisms leading to effects on the male reproductive system are largely unknown and need further characterisation. Establishing mechanisms of action and discovering potential human biomarkers will aid human risk assessment.
This project aims to identify key events of altered foetal steroid signalling, and to collect data on the current status of reproductive health of young men in Switzerland (incidence of infertility, urogenital malformations, testicular cancer). Linking mechanisms of altered foetal steroid signalling to epidemiological data will enable the identification of potential human biomarkers of exposure and effect, and thus contribute to human risk assessment and early identification of new male reproductive toxicants.
Contact
Prof Serge Nef
serge.nef@unige.ch
University of Geneva, Molecular and developmental biology of sexual development
Publications
Human Reproduction , 18 Jun 2021
The L1-dependant and Pol III transcribed Alu retrotransposon, from its discovery to innate immunity
Molecular Biology Reports , 31 Mär 2021
Andrology , 13 Mär 2020
WP1 – DNA methylation in mice and humans
Rationale for the project
An in vivo mouse model has been developed for precise evaluation of epigenetic changes, such as DNA methylation, in sperm, as well as for evaluation of reproductive performance after exposure to toxic compounds. The experimental results suggest that the deleterious effects of compounds with endocrine disruptor properties on the male reproductive system are accompanied by methylation defects in sperm DNA. These were found to be present in the exposed animals but also in the progeny of the exposed generation, meaning a transgeneration germline-inheritable deleterious effect. These results support the hypothesis of a link between exposure to endocrine disruptors and male infertility.
Objectives
The objective of this project is to assess whether DNA methylation changes may be considered as a biomarker of effect, and whether exposure to low-level human-relevant doses of endocrine disrupting chemicals also lead to methylation changes and defective spermatogenesis.
Partners: Christian De Geyter (University Hospital Basel), Serge Nef (University of Geneva)
Project lead
Dr Ariane Giacobino
ariane.giacobino@unige.ch

WP2 – Association between male anogenital distance, sperm phenotype and epigenetics in infertile men
Rationale for the project
During prenatal development the fetal testes undergo a number of changes in which the exact balance between male and female sexual hormones is crucial. The testicular dysgenesis syndrome (TDS) results from exaggerated exposure of the fetal testes to endocrine disruptors and consists of testicular maldescent, hypospadias, reduced sperm count and infertility during adulthood and testicular cancer. In the semen of men with TSD, a higher proportion of spermatozoa may carry epigenetic abnormalities which can be transmitted to their offspring and impair long term health. Shortened anogenital distance (AGD) is thought to be an appropriate clinical marker of TDS.
Objectives
The project aims at identifying the relationship between male infertility, shortened AGD and epigenetic abnormalities of selected subpopulations of spermatozoa. Methods are being developed to identify subpopulations of human spermatozoa with decondensed chromatin and/or fragmented DNA, aiming at separating these from normal spermatozoa using flow cytometry and sorting (FACS). After sorting, differences in the epigenetic methylation state and histone content of the sorted populations of spermatozoa will be compared in infertile men with shortened AGD and in fertile semen donors with normal AGD.
Partners: Ariane Giacobino (University of Geneva), Ludwig Stenz (University of Geneva)
Project lead
Prof Christian De Geyter
christian.degeyter@usb.ch
University Hospital Basel, Reproductive medicine and gynecological endocrinology


WP3 – Assessment of male fertility in Switzerland
Rationale for the project
Male reproductive health has been declining over the past decades in many European countries. The drop of semen quality occurs over a short timescale which suggests that the causes are lifestyle and environmental rather than genetics. In Switzerland, no information is available on male reproductive health including semen parameters and exposure to endocrine disruptor chemicals (EDCs). A large-scale epidemiological study on the male reproductive health in Switzerland was therefore launched to collect data on 3000 military conscripts from all regions of the country during their visit to the national army’s recruitment centers.
Objectives
The goals are to complete data collection on the 3000 conscripts and to provide the first large scale study on male reproductive health in Switzerland. More precisely, epidemiological studies will be performed to investigate how reproductive parameters such as sperm quality and hormones could be influenced by lifestyle (e.g. tobacco, alcohol, recreational drugs) and environmental factors (e.g. exposure to endocrine disruptors, geographical parameters, occupational factors).
Partners: Niels Joergensen (University of Copenhagen), Luc Multigner (University of Rennes), Michel Rossie (Valais Hospital), Serge Rudaz (University of Geneva), Alfred Senn (University of Geneva), Eric Stettler (Swiss Army)
Project lead
Prof Serge Nef
serge.nef@unige.ch
University of Geneva, Molecular and developmental biology of sexual development


WP4 – Human key event readouts related to male infertility
Rationale for the project
Reproductive toxicants may contribute to a spectrum of adverse effects on male reproductive health such as decreasing sperm quality, decline in serum testosterone, increase in testicular cancer incidence, and infertility. These adverse effects observed in adult individuals may result from exposure at various key stages of human development from the embryo to adulthood. The relationship between hormone alterations and reduced male fertility triggered by environmental chemical exposure during development and adulthood will be investigated using in vivo steroid analysis. Because of the pivotal role of androgenic signalling in spermatogenesis, altered steroid profiles are hypothesised to be a key event leading to reduced male fertility. The tests in adults will be performed on a cohort composed of Swiss army conscripts.
Objectives
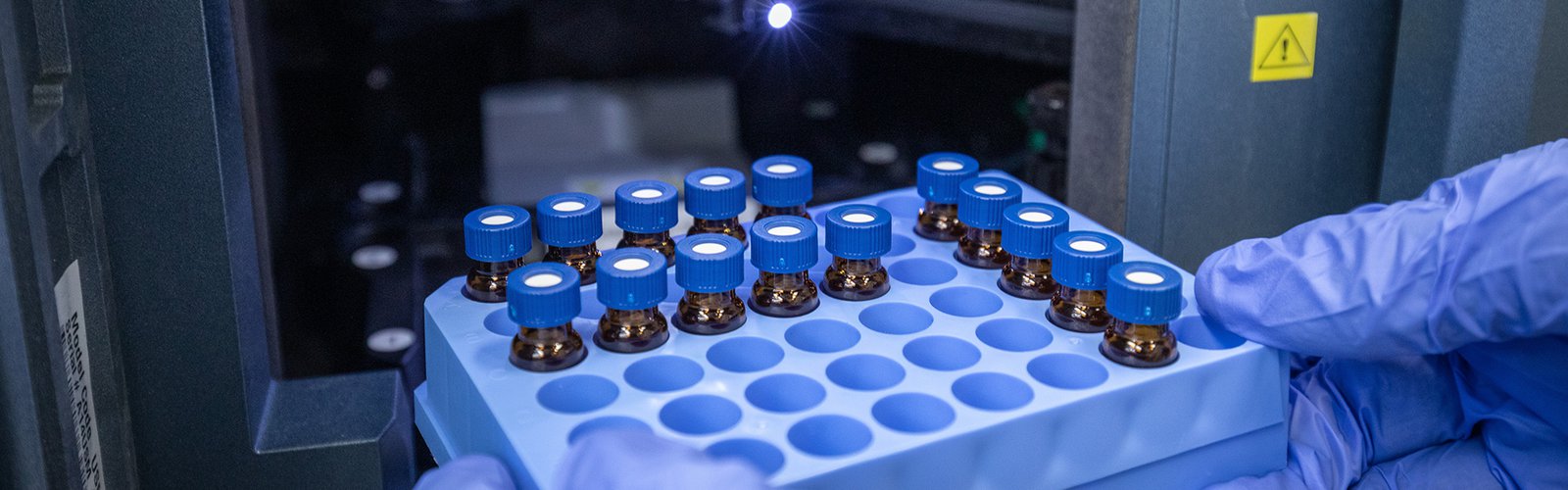
Untargeted steroidomics, as a metabolomics-based approach, is a method of choice to evaluate extended steroid profiles. Furthermore, untargeted acquisition may lead to discovery of new unknown key event readouts that can provide complementary information to the measured steroids. In comparison to classical steroid analysis, steroidomics require specific development for sample preparation, highly efficient separation and detection. The obtained extended steroid profile will help to provide information on putative key events leading to male infertility. Steroidomics data will be obtained by Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS); identification of molecules is based on measured mass to charge ratio (m/z) of steroid ions and their fragment ions after collision in the mass spectrometer (MS/MS spectra).
Partners: Serge Nef (University of Geneva), Michel Rossier (Valais Hospital)
Project lead
Prof Serge Rudaz
serge.rudaz@unige.ch
